Bodyfeeding: History of chest surgery
Planning for chest surgery
Gender affirming chest surgeries will, in most cases, impact the person’s ability to make milk and bodyfeed an infant. This should be included in the surgical consent process before chest reduction or construction surgery.
Chest reduction or construction surgery is pursued by some transgender, Two-Spirit A term used within some Indigenous communities to reflect complex Indigenous understandings of gender and sexuality and the long history of sexual and gender diversity in Indigenous cultures. Two-Spirit encompasses sexual, gender, cultural and spiritual identity. It may refer to cross-gender, multi-gender or non-binary gender roles, non-heterosexual identities, and a range of cultural identities, roles and practices embodied by Two-Spirit peoples. Some people also use "2-Spirit" or "2S." (Source: Battered Women’s Support Services) , and non-binary Umbrella term referring to people whose gender does not fall within the binary gender system of woman/girl or man/boy. Some individuals identify as non-binary while others may use terms such as gender non-conforming, genderqueer, or agender. Non-binary people may or may not conform to societal expectations for their gender expression and gender role, and they may or may not seek gender-affirming medical or surgical care. (TTNB) people to align their physical appearance with their gender. For TTNB people who can become pregnant, gender affirming chest surgery may make pregnancy a viable option to grow their family [1]. Some people who have had gender affirming chest surgery will want to bodyfeed their infants.
While there is no way to know how surgery will impact someone’s milk supply until they attempt to bodyfeed, most people who have had gender-affirming chest surgery will have decreased milk production [2].
Beyond nutrition, bodyfeeding allows for bonding and has benefits for the parent and infant, regardless of the amount of milk produced. The client’s goals and desires should remain the central focus when supporting infant feeding after chest surgery. Ensuring clients have adequate support is a key factor in achieving bodyfeeding goals after chest or breast surgery (Mitchell, 2022).
Milk production
Milk production is multi-faceted and impacted by many different factors (e.g., personal health history, social supports), one of which is the structure and tissue of the chest or breast. It is difficult, therefore, to know how chest or breast surgery will impact each client’s ability to produce milk [3]. Some sources state that bodyfeeding and producing milk is impossible after a complete chest reconstruction [2], however, there are cases of people who have produced a small amount of milk and bodyfed for years using a supplemental feeding system [4].
This overview of surgery types is not intended to be exhaustive. It aims to provide an overview of surgical methods to support providers to engage in informed feeding discussions with clients who are exploring bodyfeeding after chest surgery.
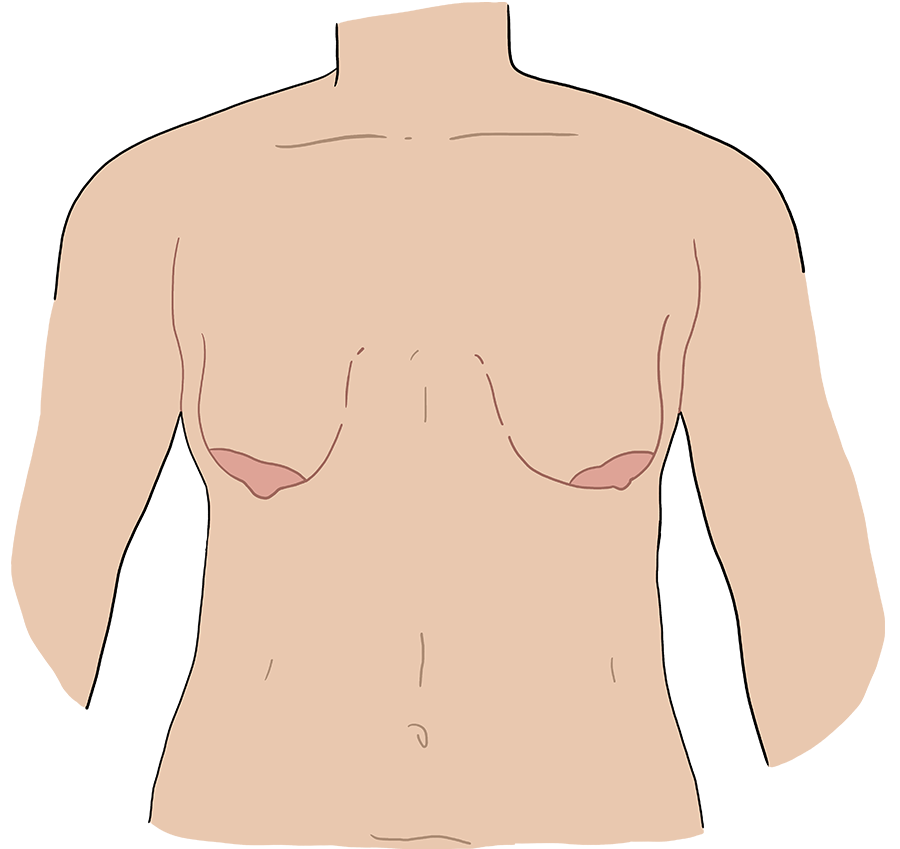
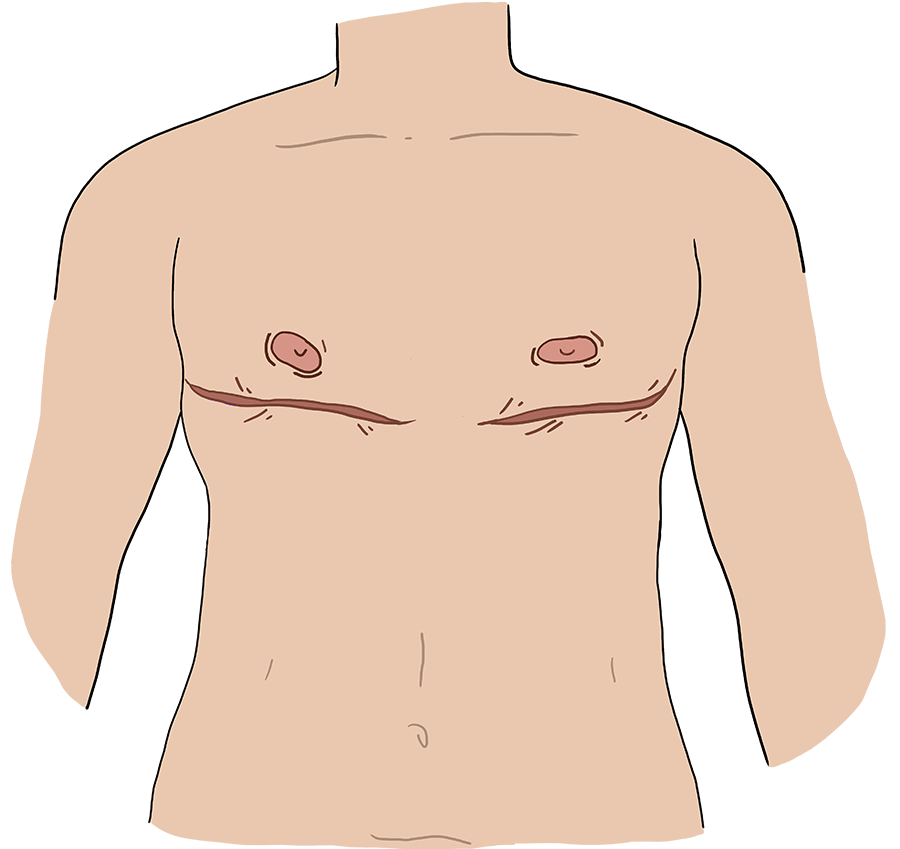
Keyhole A surgical approach where an incision is made around half the outer edge of the areola (the darker area surrounding the nipple) to access underlying tissues or perform procedures. incision
A small incision is made at the lower border of areola, removing underlying tissue but not excess skin [5].
- Suitable for those who have a smaller amount of chest tissue with high skin elasticity.
- Nipple-areolar complex pedicle remains intact, goal to maintain some nipple sensation, but a transient or permanent diminished sensation is a common side effect.
- Some nipple reduction may be performed, but the nipples are typically not repositioned (this could be addressed in a separate procedure if needed).
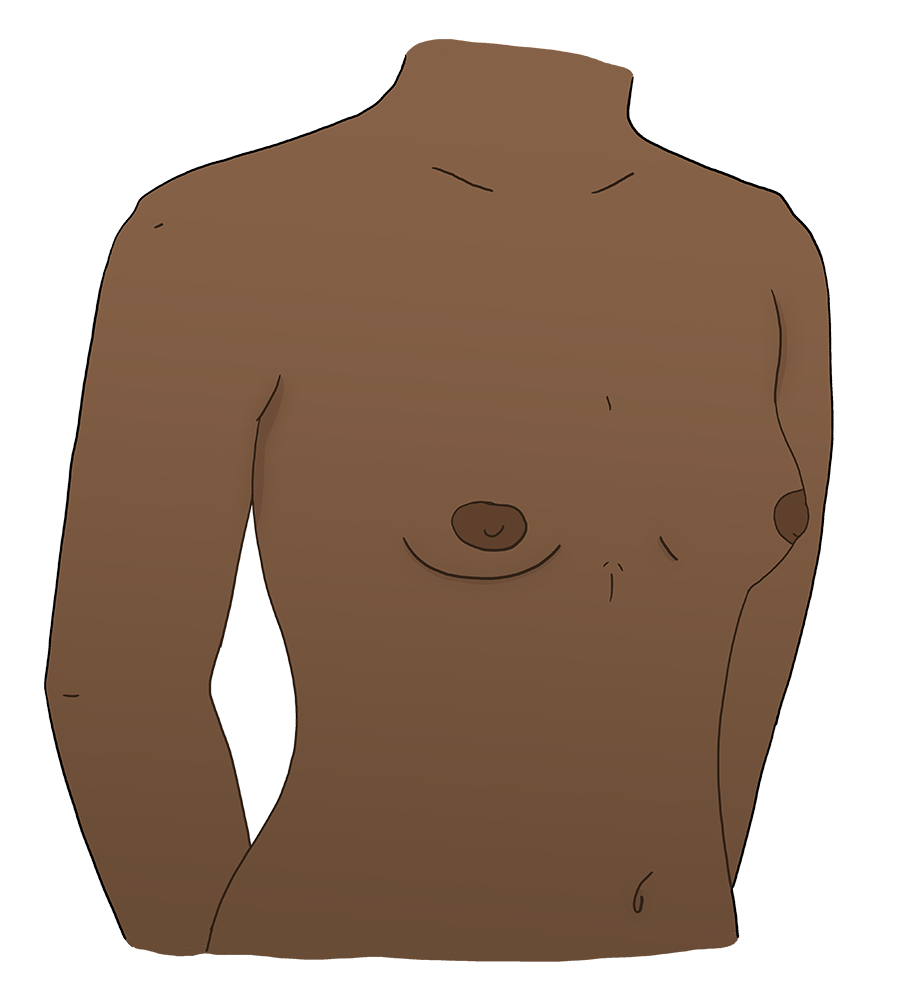
Before
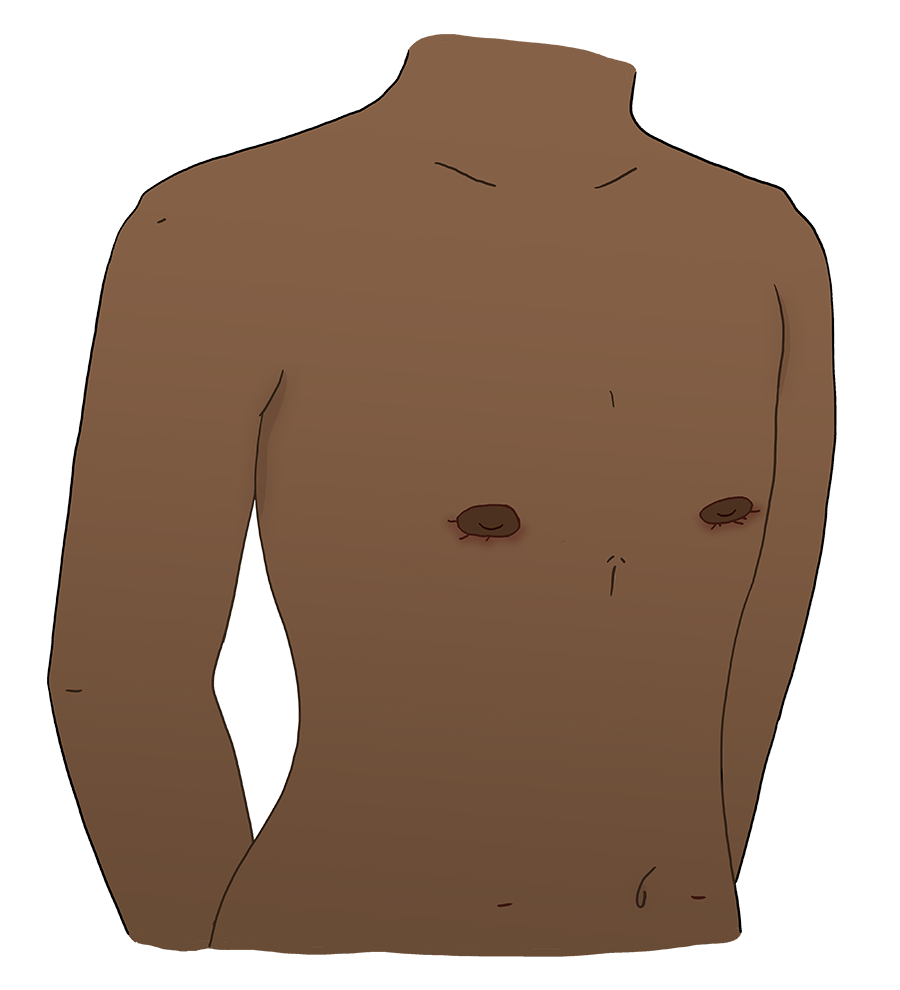
After
Periareolar A surgical approach where an incision is made around the outer edge of the areola (the darker area surrounding the nipple) to access underlying tissues or perform procedures. incision
Circular incisions are made around the areola, and a donut-shaped area of skin is removed from around the areola. Excess skin and tissue are removed through the incisions, and the remaining skin is drawn in towards the aerolas and sutured in place [5].
- Suitable for those who have a smaller amount of chest tissue with high skin elasticity.
- Nipple-areolar complex pedicle remains intact, goal to maintain some nipple sensation, but a transient or permanent diminished sensation is a common side effect.
- Some nipple reduction may be performed, but the nipples are typically not repositioned.
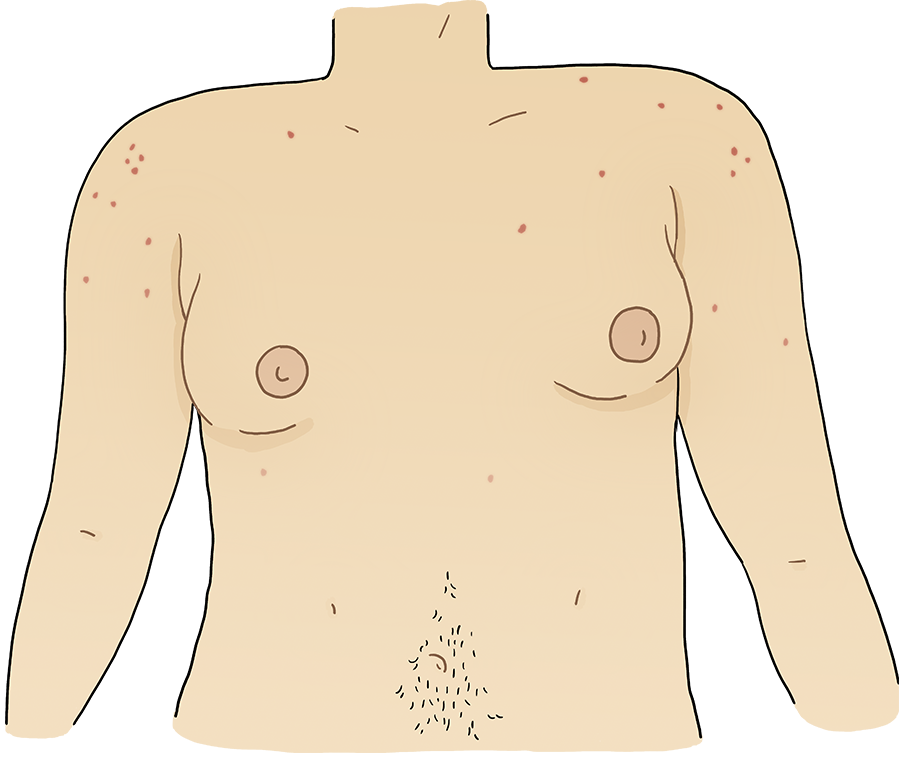
Before
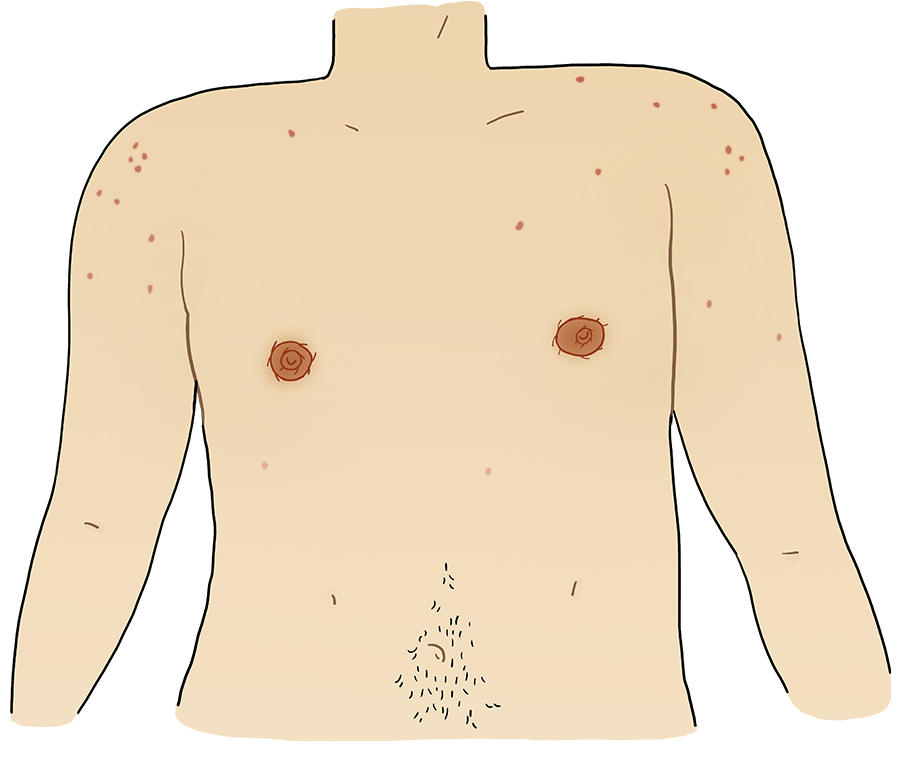
After
Double incision A surgical technique used in gender-affirming chest surgery where two horizontal incisions are made along the bottom border of the pectoral muscles. Nipples may or may not be grafted onto the chest.
Two horizontal incisions are made below the lower border of the pectoral muscle and nipples are removed. Chest tissue, fat, and skin is removed between the incisions, including the nipple-areolar complex pedicle, while ensuring the chest maintains a natural contour. The nipple-areolar complex is removed, resized, and grafted back onto the chest as free nipple grafts [5].
- Suitable for individuals with a moderate to large amount of chest tissue or more skin laxity.
- The nipple-areolar complex is removed, resized, and grafted back onto the chest as free nipple grafts.
- This typically results in no nipple sensation being preserved.
- In some cases, the nipple-areolar complex may be resized but left attached to the pedicle to potentially retain some nipple sensation, but a transient or permanent diminished sensation is a common side effect.
Before
After
Inverted T incision
Incisions are made in the shape of an inverted “T”, with one horizontal incision along the chest fold and a vertical incision from the fold to the nipple-areolar complex. Chest tissue, fat, and skin is removed, creating a flatter or smaller chest contour. The nipple-areolar complex pedicle remains intact, with the goal to maintain some nipple sensation. The nipple-areolar complex is typically resized and repositioned [5].
- Suitable for individuals with a moderate to large amount of chest tissue or more skin laxity.
- Nipple-areolar complex pedicle remains intact, goal to maintain some nipple sensation, but transient or permanent diminished sensation is a common side effect.
- Some nipple reduction and repositioning is usually be performed.
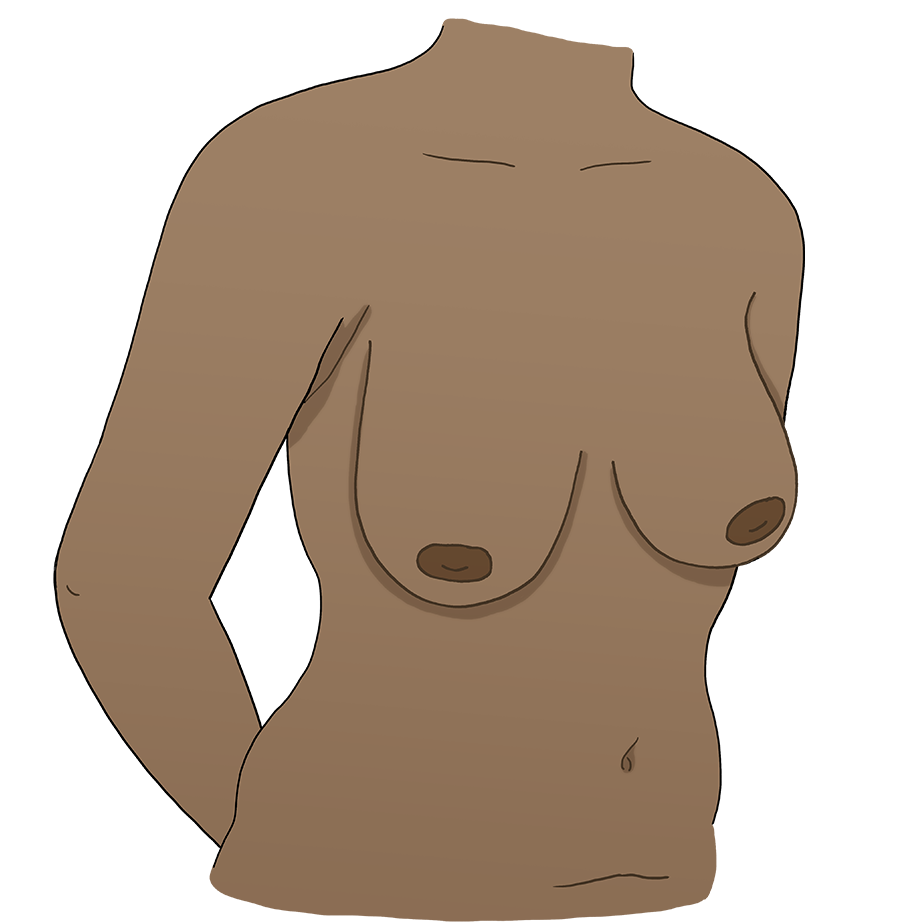
Before
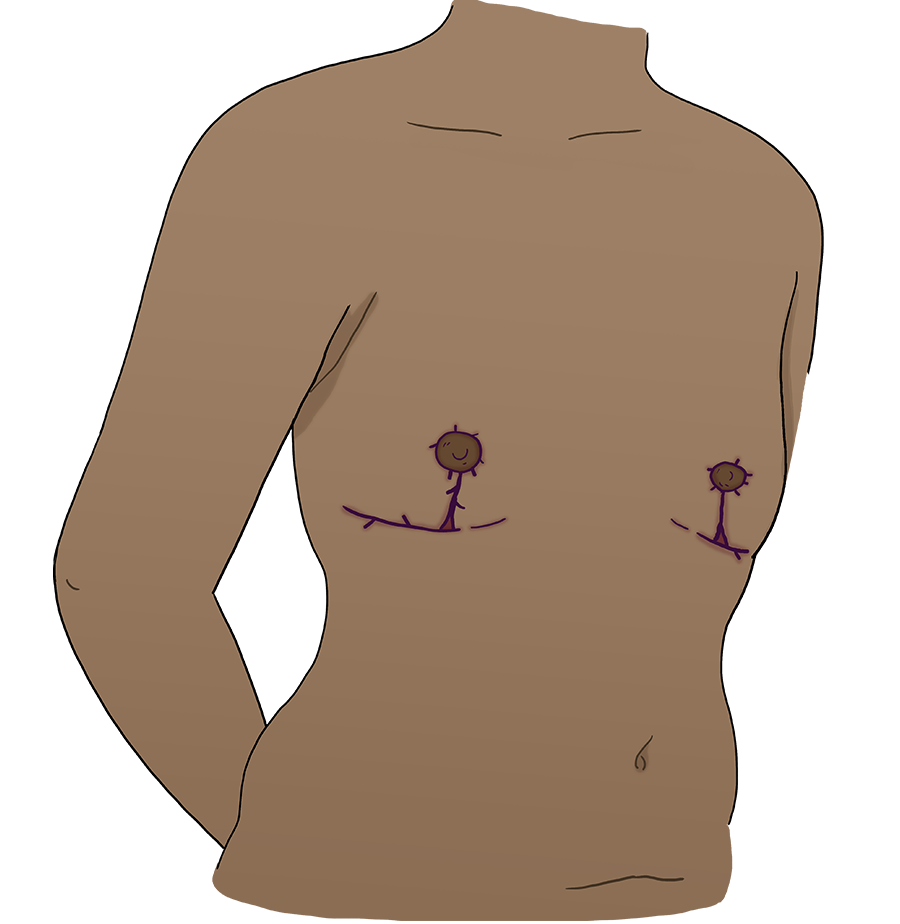
After
Fishmouth incision
Curved incisions (resembling a fishmouth) are made the pectoral muscles scarring. Nipple-areolar complex pedicle remains intact, with the goal to maintain some nipple sensation. The nipple-areolar complex is typically resized and repositioned [5].
- Nipple-areolar complex pedicle remains intact, goal to maintain some nipple sensation, but transient or permanent diminished sensation is a common side effect.
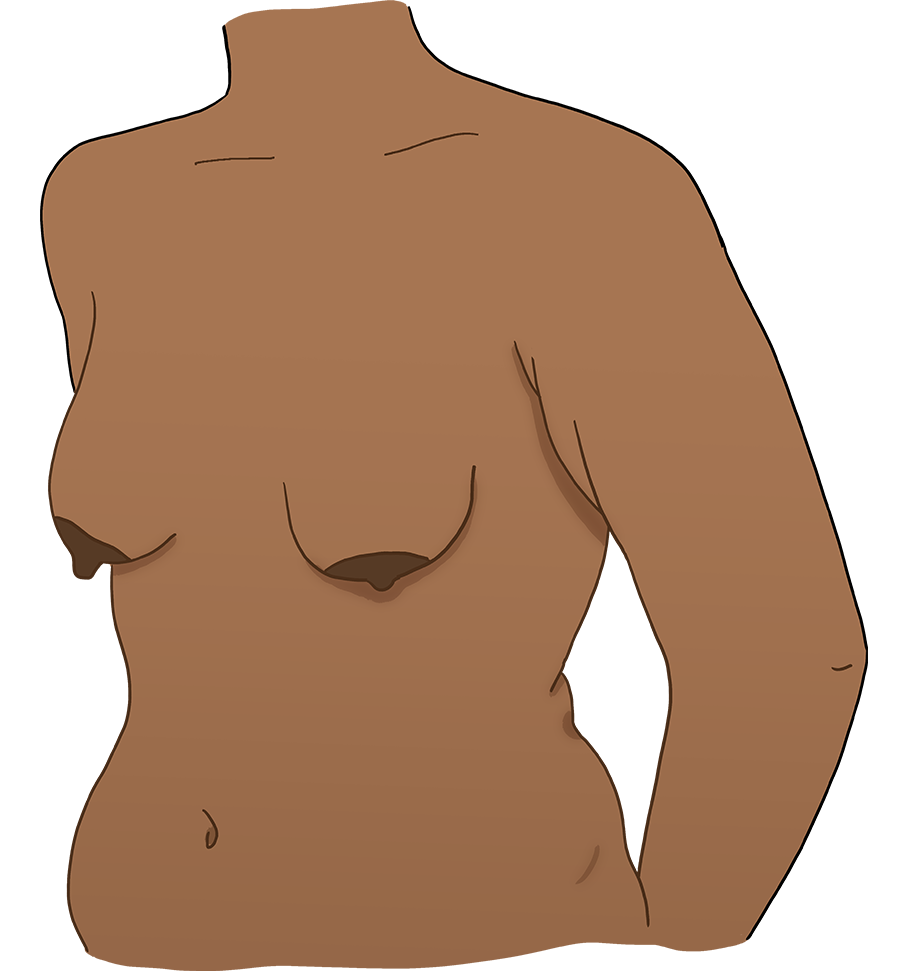
Before
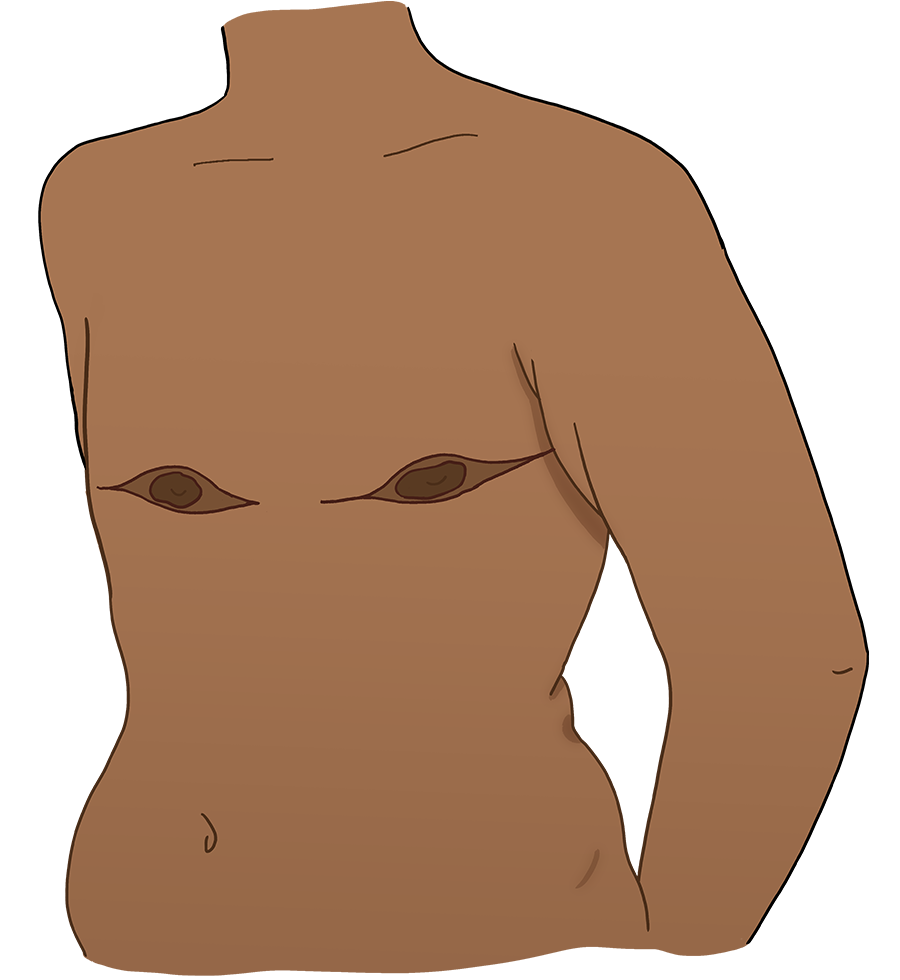
After
Accompanying client resource
Bodyfeeding after Chest Surgery
While the type of surgery may predict milk production and storage capacity, the overall impact of chest or breast surgery on nerves, blood flow, and tissue is variable and needs to be evaluated on an individual basis [6].
Nerve damage may be anticipated in some surgeries and considered an acceptable risk, in other cases, it may be an unexpected complication.
Factors that may impact milk supply
- Amount of chest or breast tissue removed may impact capacity to make and store milk.
- Chest growth during pregnancy may indicate amount of glandular tissue remaining.
- Certain medical conditions, such as insulin resistance or hormonal disorders, may impact milk production [7]. For more information, see History Taking for Infant Feeding.
- Involvement of nipple and nipple stalk in surgery or revisions:
- One qualitative study found an intact nipple stalk to be anecdotally linked with successful bodyfeeding [1].
- Surgeries that remove the nipple and graft A surgical procedure in which one section of healthy skin is removed from a part of the body and used in another location (or in the same location in the case of nipple grafts). it back onto the chest will impact milk production and may completely inhibit milk production or expression [2,8].
- If a client has bodyfed an infant since having chest or breast surgery, this experience should guide expectations rather than the type of surgery [6].
The type of surgery cannot be determined by type of scar. If the client is not familiar with the type of surgery they had and is interested in bodyfeeding, request surgical records with client’s consent.
Beyond nutrition, bodyfeeding allows for bonding and has benefits for the parent and infant, regardless of the amount of milk produced. The client’s goals and desires should remain the central focus when supporting infant feeding after chest surgery. Ensuring clients have adequate support is a key factor in achieving bodyfeeding goals after chest or breast surgery [8].
Planning for low supply
Many people who bodyfeed after chest surgery will have lower milk production. This is a variation of normal and supplementing with donor milk or formula should be expected, not framed as a failure to produce enough milk.
Discussing the possibility of a low supply after surgery is not intended to discourage clients but to allow them to make an informed decision about how much effort they want to put into feeding and how they would like to provide supplementation.
Postpartum support
Clients who are bodyfeeding after chest surgery will likely need increased support in the immediate postpartum. This may include home visits to weigh infants and provide feeding support. If you are unable to provide this level of support, discuss this with your client and help them create a plan. If referring clients elsewhere for postpartum support, ensure you are referring them to clinicians who provide gender-affirming care Processes through which a health care system cares for and supports an individual while recognizing and acknowledging their gender and expression. and are familiar with infant feeding after chest or breast surgery. Costs of private paid lactation support can be prohibitive for some clients - consider offering resources that have differing cost levels if a client is not comfortable discussing their financial situation.
Options for support in the postpartum period:
- International Board-Certified Lactation Consultants (IBCLCs): IBCLCs are specialists in providing infant feeding support. They may also be trained as a birth support worker (doula), nurse, midwife, or doctor.
- Registered Midwives (RMs): RMs may provide infant feeding support covered by the BC medical services plan (MSP The Medical Services Plan (MSP) is a B.C. government health plan that pays for physician services and referred services that are considered medically necessary, such as specialists (surgeon, psychiatrist, etc.), diagnostic x-rays, or laboratory services, for all BC residents. Some residents qualify for premium assistance for physiotherapy, chiropractic, naturopathy, massage therapy and acupuncture. ). Some RMs work as IBCLCs and offer lactation consultant services during pregnancy and up to six weeks postpartum. Other RMs provide postpartum care, including infant feeding support, for people they did not provide care to during pregnancy.
- Hospitals and Clinics: Some health care settings may offer MSP-funded IBCLC services.
- Private Lactation Consultants: If MSP-funded support is not available or clients need more support than is available, they can hire an IBCLC or private lactation consultant. Some private health benefit plans may cover this expense.
Positioning
Depending on their anatomy, certain feeding positions may be more comfortable for clients who have had chest surgery. If the chest tissue and skin is taut, any positions that stretch out the skin (side lying, laid back) will make it difficult for their infant to latch. Forward leaning positions may increase the amount of tissue available for latching.
Galactagogues
Non-pharmacological and pharmacological galactagogues should only be considered once there is evidence milk can be removed once milk has come in (days 2-5 postpartum). Increasing milk supply without effective removal increases the risk for engorgement and mastitis, which can occur even if milk is not able to be expressed.
- MacDonald T, Noel-Weiss J, West D, Walks M, Biener M, Kibbe A, et al. Transmasculine Refers to trans people who were assigned female at birth and whose gender expression leans towards the masculine. individuals’ experiences with lactation, chestfeeding, and gender identity A person's deeply held, internal sense of themself as male, female, a blend of both or neither. (Source: GenderSpectrum.org) : A qualitative study. BMC Pregnancy Childbirth. 2016;16: 1–17. doi:10.1186/s12884-016-0907-y
- Mosser S. Chestfeeding. In: Gender Confirmation Center [Internet]. [cited 17 Oct 2023]. Available: https://www.genderconfirmation.com/blog/chestfeeding/
- Physician Guide to Breastfeeding. Plastic surgery and breastfeeding. 8 Sep 2022 [cited 17 Oct 2023]. Available: https://physicianguidetobreastfeeding.org/surgery-and-breastfeeding/plastic-surgery/
- MacDonald T. Where’s the mother: Stories from a transgender dad. Winnipeg: Trans Canada Press; 2016.
- Mosser S. Types of top surgery Refers to some gender-affirming above-the-waist surgeries, including chest surgeries and breast surgeries. . In: Gender Confirmation Center [Internet]. [cited 17 Oct 2023]. Available: https://www.genderconfirmation.com/ftm-top-surgery-options/
- West D. Defining your own success: Breastfeeding after breast reduction surgery. 1st ed. Schaumburg, Ill: La Leche League International; 2001.
- Hoover KL, Marasco LA, Fornow KR. Low milk production and infant weight. Second edition. In: Lactation Education Accreditation and Approval Review Committee, Spencer B, Campbell SH, Chamberlain K, Lauwers J, Mannel R, editors. Core curriculum for interdisciplinary lactation care. Second edition. Burlington, MA: Jones & Bartlett Learning; 2022.
- Mitchell KB. Breast pathology. Second edition. In: Lactation Education Accreditation and Approval Review Committee, Spencer B, Campbell SH, Chamberlain K, Lauwers J, Mannel R, editors. Core curriculum for interdisciplinary lactation care. Second edition. Burlington, MA: Jones & Bartlett Learning; 2022.
| Current version | January 14, 2025 | |
| Authors | Caitlin Botkin | Nurse Educator, Trans Care BC; Registered Midwife (non-practicing) |
| Rowan McNiven Gladman | Registered Midwife, IBCLC | |

